Reading time: 6 min.
| An updated consensus statement from the American College of Sports Medicine: Exercise/physical activity in individuals with type 2 diabetes
An updated consensus and recommendations on exercise and type 2 diabetes (T2D) by the American College of Sports Medicine (ACSM) and the American Diabetes Association (ADA) suggested that various types of physical activity (PA) can greatly enhance the health and glycemic management of individuals with T2D.
Takeaway
This updated comprehensive consensus statement and recommendations on exercise and physical activity (PA) in individuals with T2D propose that:
- Individuals should engage in PA regularly to reduce sedentary behavior, including breaking up the sitting time with frequent activity breaks.
- Any activities undertaken with acute and chronic health complications, related to diabetes would require accommodations to ensure safe and effective participation.
- Different types of PA (flexibility and balance exercise in adults) enhance health and glycemic management in individuals of all ages with T2D.
- Barriers and inequities in PA, exercise adoption, and maintenance need to be addressed to maximize participation.
Why this matters
- In the last decade, research on exercise in individuals of different age groups with T2D has been published, while diabetes prevalence has continued to expand worldwide.
- Thus, these consensus statements provided a summary of the current evidence, along with extension and updates of the prior 2010 recommendations.
Key highlights
Exercise/PA with and without weight loss
Dietary restriction and increased PA are the foundations of intensive lifestyle (ILS) interventions used to induce weightloss.
Individuals at high risk of T2D with low PA levels benefit the most from moderate-intensity walking and other exercise with minimal weightloss.
Impact of exercise/PA on diabetes management and health risks
Multiple types of PA enhance health and glycemic management in individuals with T2D.
Regular training with aerobic exercise improves insulin sensitivity, lipids, blood pressure, other metabolic parameters, and fitness levels, even without weight loss.
Higher intensities of aerobic training are considered superior to low-intensity trainings.
Blood glucose levels and insulin sensitivity in overweight/obese adults and insulin resistance, prediabetes, or T2D were similarly improved with different structured physical training approaches, when energy expenditure is matched.
Mental health and cognition benefits
of PA
Regular PA has psychological and cognitive function benefits on individuals with T2D.
Studies suggested that regular exercise might improve psychological well-being, including health-related quality of life and depressive symptoms, in individuals with T2D.
PA recommendations for individuals
with T2D
Recommendations for adults of all ages are similar unless comorbid health conditions or older age impacts their ability and modifications are needed.
Recommended type of exercise trainings are specified in the embedded document below.
Adults and older adults
Adults with T2D should follow ≤2 consecutive days between bouts due to the transient nature of exercise-induced improvements in insulin action.
Interventions that combine aerobic and resistance training might be superior to either one alone.
Adolescents and youth
PA goals recommended for youth and adolescents with T2D are same as for youth in the general population.
Exercise (home or gym-based) and weight management programs should be encouraged for youth with T2D to enhance insulin sensitivity and cardiometabolic function and manage overweight and obesity.
Pre-exercise evaluation and training
Individuals participating in low- to moderate-intensity PA, pre-exercise medical evaluations is needed if symptoms of cardiovascular disease or microvascular complications exist.
In sedentary adults, medical clearance is recommended before participation in moderate- to high-intensity PA.
Management of acute and chronic health complications with PA
Exercise-related hypoglycemia and hyperglycemia are primary concerns around PA initiated by individuals with T2D and exercising with diabetes related chronic health complications might require accommodations to ensure safe and effective PA participation.
Exercise timing and dietary considerations
Studies have optimized timing of exercise around meals and in general to maximize blood glucose management and other health benefits in T2D.
Prevention or delay of T2D can be achieved with regular PA and maintenance of a healthy body weight, and they should focus on the amount and timing of carbohydrate intake along with an active lifestyle.
Medical interventions and exercise effectiveness
Anti-diabetes medications are co-prescribed with exercise for management of T2D. In adults with T2D, normal reduction in postprandial glycemia with metformin may be attenuated by exercise.
Glucagon-like peptide 1 agonists may improve HbA1c levels and fasting glycemia following aerobic exercise training in adults with T2D, but findings have been confounded by significant weight loss.
Barriers to adoption of PA and inequities
Barriers to physical activity participation are similar among individuals with and without diabetes and include lower self-efficacy, inappropriate goal setting, lack of access to facilities, lack of supervision or social support, and inattention to cultural distinctions.
Counseling by health care professionals might be an effective source of support and supervision of exercise sessions.
Consensus statements and recommendations
- Regular aerobic exercise training improves glycemic management in adults with T2D, with less daily time in hyperglycemia and 0.5%–0.7% reductions in overall glycemia (as measured by HbA1C)
- High-intensity resistance exercise training has greater beneficial effects than low-to moderate- intensity resistance training in terms of overall glucose management and attenuation of insulin levels
- Greater energy expenditure postprandially reduces glucose levels regardless of exercise intensity or type, and durations ≥45 min provide the most consistent benefits
- Small “doses” of PA throughout the day to break up sitting modestly attenuate postprandial glucose and insulin levels, particularly in individuals with insulin resistance and a higher body mass index
- Weight loss (accomplished through lifestyle changes in diet and PA) of >5% seems to be necessary for beneficial effects on HbA1C, blood lipids, and blood pressure
- For reductions in visceral fat in individuals with T2D, a moderately high volume of exercise (approx. 500 kcal) done 4–5 days/week is needed
- In youth with T2D, ILS interventions plus metformin have not been superior to metformin alone in managing glycemia
- Despite the limited data, it is still recommended that youth and adolescents with T2D meet the same PA goals set for youth in the general population
- Pregnant women with and without diabetes should participate in at least 20–30 min of moderate-intensity exercise most days of the week
- Individuals with T2D using insulin or insulin secretagogues are advised to supplement with carbohydrate (or reduce insulin, if possible) as needed to prevent hypoglycemia during and after exercise
- Participation in an exercise program before bariatric surgery may enhance surgical outcomes, and after surgery, participation confers additional benefits
Expert interpretation and key future directions
- Large scale clinical trials in type 2 diabetes (T2D) are required to understand optimal treatment regimens and importance of physical activity (PA) and exercise, other lifestyle changes, and medications on glycemia
- Further work is warranted to elucidate the cognitive domains that are most responsive to PA and dietary improvements in adults with T2D, effect of exercise on memory and cognitive function related to glycemic management
- More research on the effect of exercise training on vascular function and the microbiome to be conducted in individuals with obesity and with and without T2D
- Longer-duration training is needed to establish whether exercise timing modifies the glycemic response to meals as well as overnight levels and if specific time of day of planned exercise should be prescribed
- Studies on PA breaks in daily life are necessary to determine whether long-term use has clinically relevant glycemic benefits in T2D population
- Potential interactions between diabetes medications like metformin and exercise training need to be further investigated for their impact on glycemic management
- Association of social and environmental factors with physical inactivity and the incidence of T2D need to be explored further
- Research to define the health disparities across racial, ethnic, and potentially socioeconomic populations and how their impact on PA participation for T2D and prediabetes prevention and management can be mitigated needs to be studied
- Larger clinical trials examining the impact of chronic high-intensity exercise on mitochondrial function and glucose tolerance in a population with obesity and with and without T2D are needed
Recommended types of exercise training for all adults with T2D
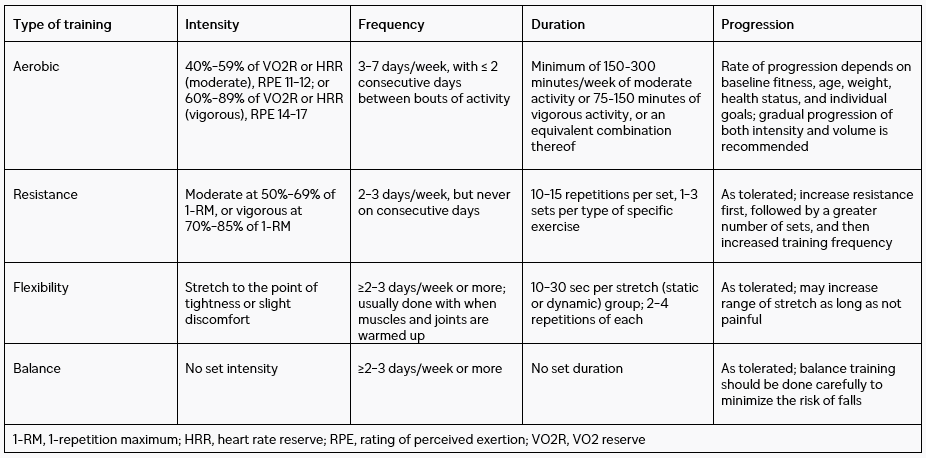
Please refer to the source publication Kanaley JA, et al. for additional details
1. Kanaley JA, Colberg SR, Corcoran MH, Malin SK, Rodriguez NR, Crespo CJ, et al. Exercise/physical activity in individuals with type 2 diabetes: A consensus statement from the American College of Sports Medicine. Med Sci Sports Exerc. 2022;54(2):353-368. doi: 10.1249/MSS.0000000000002800. PMID: 35029593.
MAT-DK-2300557 v.1.0 22.11.2023