Reading time: 3 min.
| The T1DEXI study: A Type 1-Diabetes and Exercise Initiative
This real-world study revealed that all 3 forms of home‑based exercise led to significant decrease in glucose levels, with aerobic exercise having the greatest impact and improved time in range (TIR) over the next 24-h compared to non-exercise days.
Takeaway
This study examined acute glycemic effects of at-home exercises in adults with type 1 diabetes (TID) for 4 weeks in real-world setting.
- Glucose decline during structured at-home exercise was highest with aerobic, followed by high-intensity interval and resistance exercise
- Factors influencing glucose change included pre-exercise glucose concentration, sex, glycated hemoglobin (HbA1c), pre-exercise heart rate, exercise time of day and on-board insulin level
- Structured exercise increased daily TIR by 6%, but also increased 24-h time below range (TBR), even with closed-loop insulin delivery systems
Glucose response to exercise is influenced by several factors at the event and participant level, which may need to be considered when developing new automated insulin delivery systems for T1D.
Why this matters
Hypoglycemia is identified as one of the barriers to engagement in regular exercise for adults living with T1D.
- People with T1D have varying glucose responses to regular advised exercise
- Impact of various factors such as exercise type, carbohydrate intake, insulin level, and hormone levels remain unclear*
To address this, a large ‘at-home’ observational study was conducted to examine the effects of structured exercise on glycemia using continuous glucose monitors, across patient characteristics.
- The data gathered from this study will help in the development of new adult specific T1D exercise management guidelines and improve automated insulin delivery system algorithms
Study design
- T1DEXI (Type 1 Diabetes and Exercise Initiative)– a real-world, observational study with adult T1D participants (≥18 years), randomly assigned to complete 6 sessions of ‘at-home exercises’ (aerobic, interval, or resistance) over 4 weeks.
- Participants used custom smartphone application to self-report both study and non-study exercise, food intake, and insulin dosing (multiple daily injections [MDI] users) along with pump data, heart rate and continuous glucose monitoring data.
- Study outcomes: Primary outcome was mean change in glucose level during exercise; Secondary outcome† was to compare glycemic outcomes between exercise (active) and sedentary days.
Key results
Of 561 adults with T1D, 497 were assigned to structured exercises: Aerobic (n = 162), interval (n = 165), and resistance (n = 170) exercise.
- Mean age, (range): 37 (18–70) years; Females and males, (n): 363 and 134
- HbA1c, (mean ± SD): 6.6 ± 0.8% (49 ± 8.7 mmol/mol)
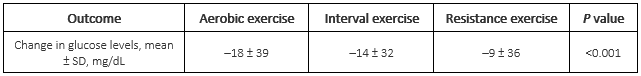
Mean change in glucose levels during assigned exercise:
- Greater decline in glucose levels with aerobic exercise compared with interval and resistance exercise, irrespective of insulin delivery mode
Factors associated with greater glucose decline during exercise (from baseline):
- Participant-level factors: Lower HbA1c levels (<7%) during baseline; Males
- Event-level factors: Higher baseline glucose (P <0.001); Declining glucose before exercise (P <0.001); Greater percent time <70 mg/dL in the 24-h before exercise (P = 0.03); Lower baseline heart rate (P = 0.02); Afternoon/evening exercise (P <0.001); Greater amount of insulin on board at the start of exercise (P <0.001)
Glycemia on exercise vs sedentary days:
- Lower mean glucose levels (mg/dL) in study exercise days (145 ± 31)§ vs sedentary days (155 ± 35)§ (P <0.001)
- Mean TIR 70–180 mg/dL was 6% higher during the 24-h after study exercise (76 ± 20)§ than sedentary days (70 ± 23)§ (P <0.001)
- Lower median percent time >180 mg/dL in exercise days (17 [5–32]) than sedentary days (23 [9–41]) (P <0.001)
- Increased 24-h TBR by all three exercise types, even with HCL insulin delivery systems
Key limitations
Reference Cohort not representative of general population with T1D; MDI users underrepresented; Assigned exercise types may not have differed much on energy systems or hormonal responses which could profoundly impact glycemia; Peak heart rate during interval exercise was lower than expected.
*Other variables include sex, fitness level, insulin delivery modality, and recent glycemic control; †Study exercise day was defined as a 24-h period after the end of a study exercise session, whereas a sedentary day was defined as a 24-h period without any exercise (study or personal) in current or past 24-h; §mean ± SD. Please refer source publication Riddell MC, et al. for additional details.
1. Riddell MC, Li Z, Gal RL, Calhoun P, Jacobs PG, Clements MA, et al. Examining the acute glycemic effects of different types of structured exercise sessions in type 1 diabetes in a real-world setting: The type 1 diabetes and exercise initiative (T1DEXI). Diabetes Care. 2023;46(4):704–713. doi: 10.2337/dc22-1721. PMID: 36795053.
MAT-DK-2300555 v.1.0 22.11.2023